Thank you for Subscribing to Healthcare Business Review Weekly Brief
Sleep disorders are rarely isolated conditions. Obstructive Sleep Apnea (OSA), arguably the most prevalent and chronically underdiagnosed sleep disorder, is deeply intertwined with broader systemic dysfunctions like cardiometabolic issues, craniofacial structural imbalances, neurocognitive deficits, and obesity. Despite OSA’s multifactorial nature, the care ecosystem surrounding OSA remains compartmentalized. Traditionally, physicians handle diagnosis and medical management, while dentists step in to offer oral appliance therapy for patients who cannot tolerate continuous positive airway pressure (CPAP) treatment. This lack of coordination and communication across specialties often leads to delays, conflicting guidance, unnecessary repeat testing, and fragmented patient experiences. Dedicated Sleep addresses these patients’ care issues by restructuring the coordination of sleep care. “Patients don’t fall through the cracks because of bad medicine. They fall through because no one is holding the thread across touchpoints,” says Jill Glenn, Founder and CEO of Dedicated Sleep. Dedicated Sleep’s multidisciplinary model connects the fragmented points of care. By aligning screening, diagnosis, therapy and long-term support within a single pathway, Dedicated Sleep ensures patients are not left on their own to navigate disconnected steps. A patient who is struggling with CPAP, or another patient who begins with a dental screening or home sleep study, is guided into the same continuum of care. Physicians, dentists and other providers work in tandem rather than in silos. Each handoff of the patient by healthcare professionals reinforces the clinical direction, allowing treatment plans to adjust as patient needs evolve. Dedicated Sleep’s model is clinically effective due to its layered expertise, supported by healthcare professionals from diverse backgrounds in pulmonary, craniofacial, behavioral health and dental sleep medicine. This comprehensive model enables nuanced evaluation and shared decision-making, which is critical when managing complex, chronic conditions like OSA, because symptoms and root causes often overlap across multiple systems. “We’ve built a care architecture that respects the patient’s time and the complexity of their condition,” Glenn explains. “When people come to us, they’re often tired, not just from sleep deprivation, but from the runaround. What we offer is a system that’s clinically sound, emotionally reassuring and structurally complete.”...Read more
Top Healthcare Consulting Service 2025
Today’s healthcare landscape is often defined by operational and financial intricacies, making the need for organizations that can diagnose the root causes of such issues more critical than ever. Under CEO Matthew Punches’ leadership, Punches Consulting precisely addresses this need. It helps healthcare groups optimize their operations and revenue cycle management (RCM) through a candid, data-driven approach, transforming ambiguous concerns into clear strategic insights, financial... Read more
Top Medical Assistant Continuing Education Service 2025
ANNALS of CONTINUING EDUCATION (ACE) is a web-based platform that supports medical assistants (MAs) across all disciplines by providing affordable, accessible, and high-quality continuing education units (CEUs). ACE’s mission is to enhance professional growth, elevate patient care, and empower healthcare careers through flexible and cost-effective learning. With an annual membership offering unlimited courses for just $49.95, ACE removes financial and logistical barriers for the r... Read more
Top Psychological Services 2025
Think of this scenario: You finally start to feel a sense of trust taking shape between your therapist and you. After weeks of opening up about what keeps you awake at night, something begins to shift. Mornings feel calmer and the spirals are less frequent. Then your therapist says, “You’ve made real progress with your anxiety, but the tension in your relationship might be better addressed with a specialist in interpersonal psychotherapy.” And just like that, you’... Read more
CXO INSIGHTS

The Significance of a Chief Nursing Officer in Healthcare Excellence
Dawn L. Alexander, Chief Nursing Officer, DCH Health System

Physical and Psychological Impact of Reconstructive Surgery
Ernie Livingston, Director of Surgical Services, Springhill Medical Center

Tech Innovations to Improve Healthcare Processes
Audrey Neylon, System Director Mental Health & Addiction, Fairview Health

Dental Marketing: Building a Strong Brand Identity and Positive Reputation through Community Engagement
Jaclyn Nona, Marketing Manager at Restore Dental Arts

From Detective to Director: Navigating Leadership, Trust and Innovation in Modern Nursing
Richard Ortiz, Director of Patient Care Services, Hackensack Meridian Health

Navigating The Future Of Pharmacy
Amos Chery, Director, Pharmacy Operations and Regulatory Compliance, MedStar Health
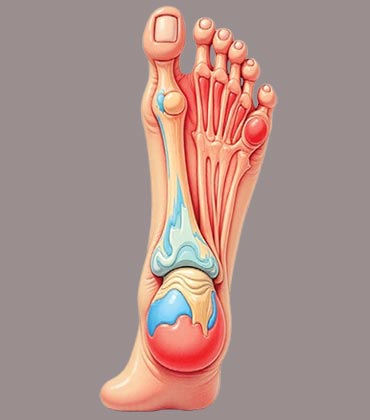
Revolutionizing Podiatry for Efficient Patient Care
Ron Guberman, Director of Podiatric Medical Education and Co-Chief of the Podiatry Division, Wyckoff Heights Medical Center
IN FOCUS
Sleep Enhancement through Customized Dental Interventions
Dental sleep care provides minimally invasive methods to enhance sleep quality, promote overall health, and improve long-term wellness.
Innovative Learning Pathways for Medical Assistants: Advancing Skills and Careers
Medical assistant continuing education strengthens skills, ensures compliance, supports career growth, leverages technology, and enhances patient care through flexible, innovative learning pathways.
EDITORIAL
Where Innovation and Integration Redefine Healthcare’s Next Chapter
But innovation doesn’t sustain itself without the right talent and mindset. Medical assistant continuing education programs are closing the skill gap, preparing clinicians to operate confidently in hybrid, data-driven environments. At the same time, psychological services are emerging as essential infrastructure that supports clinician resilience, patient adherence, and organizational performance. Together, these disciplines signal a new era in healthcare defined by integration, agility, and accountability. The systems that unify expertise across domains to deliver measurable value for patients, providers, and organizations will lead the transformation from volume-based care to value-based performance.
This edition of Healthcare Business Review spotlights leaders and organizations driving this integrated vision forward. It features those redefining standards of care, operational excellence, and patient-centered innovation across dental sleep medicine, healthcare consulting, continuing education, and psychological services.
We hope this edition inspires healthcare professionals, educators, and leaders to explore new ways of integrating expertise, data, and empathy into everyday practice. By learning from these innovators, the industry can continue to evolve toward a more connected, efficient, and humancentered model of care.